Home HOW CAN X-RAY HELP DIAGNOSE ARTHRITIS?
According to the Arthritis Society of Canada, one in five Canadians live with arthritis every day. The term arthritis applies to over 100 diseases, which most often cause inflammation in the joints. Inflammation is redness and swelling which can cause pain and stiffness in the joints.
There are two main categories of arthritis conditions:
For both categories of arthritis, the symptoms can include the following:
OA usually progresses slowly over months or years and early symptoms tend to come and go. It commonly affects the knees, hips, first toes, wrists, thumbs, fingers, and spine. As damage progresses, symptoms can become more constant, occurring at rest and disturbing sleep.
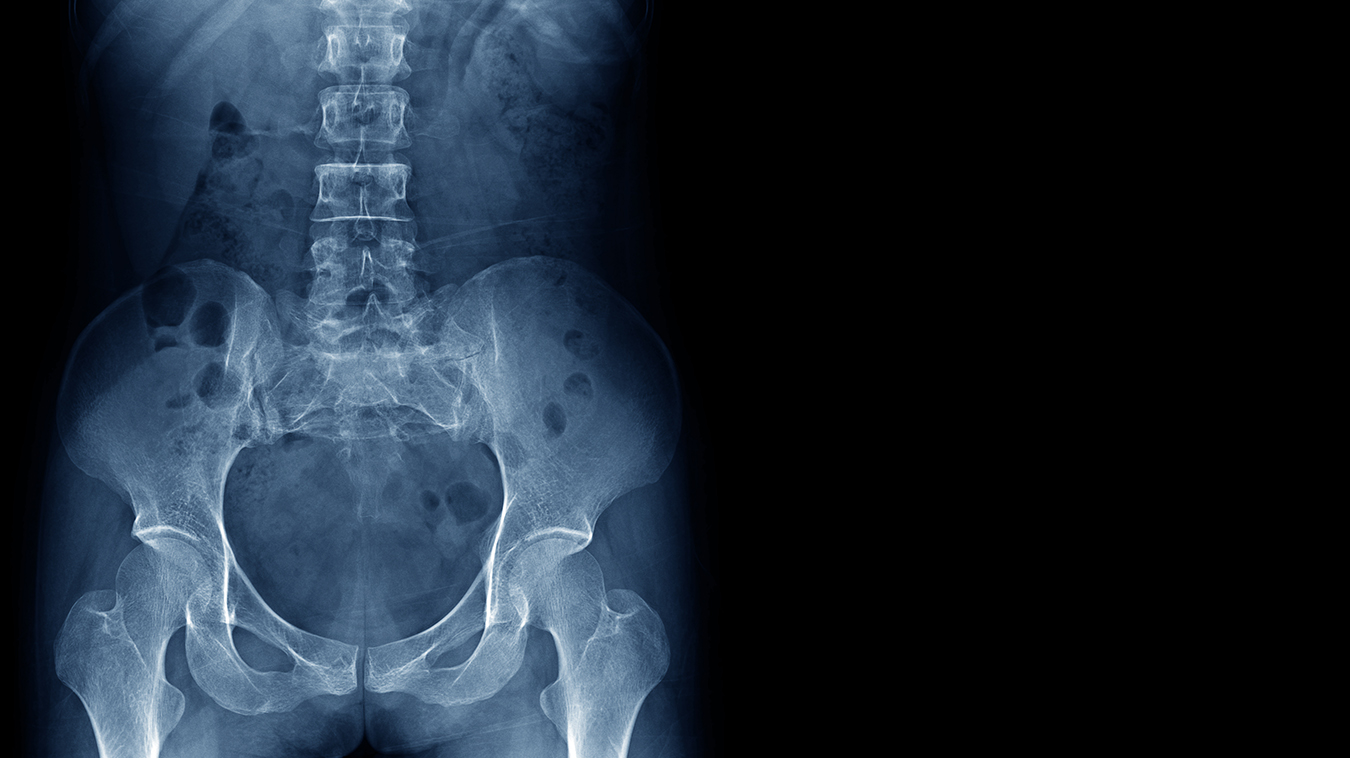
Osteoarthritis is usually diagnosed through a clinical assessment based on your symptoms and a physical examination. X-ray may be ordered to confirm the diagnosis and establish the severity of your OA. For suspected inflammatory arthritis, you will be referred to a rheumatologist, but X-ray may also be ordered to look for signs of OA or to monitor the progression of the disease.
X-ray is often the first step for imaging to investigate arthritis because its inexpensive and readily accessible. On the X-ray image, the radiologist will look for:
Magnetic resonance imaging (MRI) may also be ordered when investigating arthritis. MRI can help provide information about cartilage, tendons, and other structures in the joint, as well as showing the presence of swelling caused by too much fluid in your tissue (edema).
For osteoarthritis, treatment options can vary depending on the stage of progression of the disease. Bracing and wraps to ensure joint stability may help at any stage. In the early stages, weight loss and exercise may be recommended to slow the progression of the disease, and oral nonsteriodal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, may be ordered to help relieve pain and inflammation. Other options include:
For inflammatory arthritis conditions, some of the initial treatment options are similar to those for OA, such as exercise and weight loss or diet changes. Other treatments can include anti-rheumatic and anti-inflammatory medication, as well as cortiocosteriod injections.
Arthritis conditions are chronic (long-term) and, although there is no cure, treatment can help reduce your symptoms and make it possible for you to lead a full and active life. Studies suggest treatment in early stages of the disease is the most effective way to prevent progression. In most cases, you can manage mild to moderate arthritis symptoms for many years with a treatment plan. It’s also important to thoroughly discuss all your options with your health care practitioner, especially in the later stages of the disease.
For more information on pain management injections, please speak to your health care practitioner.
REFERENCES
Arthritis Society Canada (2023) “What is arthritis?” www.arthritis.ca. Accessed July 12, 2023.
Bennington-Castro, J. (2023) “What Is Osteoarthritis? Symptoms, Causes, Diagnosis, Treatment, and Prevention.” www.everyday.health. Accessed July 12, 2023.
Frank, J. (2021) “Rheumatoid Arthritis (RA) Diagnosis.” www.arthritis-health.com. Accessed July 12, 2023.
Holland, K. (2023) “Stages of Osteoarthritis (OA) of the Knee.” www.healthline.com. Accessed July 12, 2023.
Johns Hopkins Arthritis Centre (2023) “Osteoarthritis: Signs and Symptoms.” www.hopkinsarthritis.org. Accessed July 12, 2023.
We foster a supportive and collaborative culture designed to encourage positive patient experiences and build strong working relationships across the organization:
Our core values shape the way we work with patients, partners, and fellow employees. And, more than anything else, they’re what set Mayfair apart. In everything we do, this is what we strive for:
EXCELLENCE
We share a commitment to high quality and excellence in all that we do. This commitment calls on all of us to achieve the very best of our capabilities and exceed our own expectations.
CURIOSITY
We innovate in everything, from services to processes. We believe meaningful change and effective problem solving come only by looking at challenges and opportunities from new angles and by exercising our creativity and curiosity.
PASSION
We show pride, enthusiasm, and dedication in everything that we do. We are committed to producing and delivering high-quality results and services. We are passionate about our industry and about our company, services, partners, and patients.
COLLABORATION
Our team is supportive of each other’s efforts; we are loyal to one another; and we care for one another both personally and professionally. We promote and support a diverse, yet unified, team. We work together to meet our common goals across Mayfair clinics, locations, and geographies. Only through collaboration on ideas, technologies, and talents can we achieve our mission and vision.
SERVICE
We take pride in delivering exceptional service every day. We listen to every request with an open mind, always looking for opportunities to go above and beyond to create memorable, personalized experiences. We take responsibility to answer our referrers’ and patients’ requests and respect their time by always responding with a sense of urgency.
Start a career with Mayfair Diagnostics — one of Western Canada’s leading medical imaging teams.
Headquartered in Calgary, Alberta, we’ve been helping people f ind clarity for their health for over 100 years. At our clinics in Calgary and area, Regina, and Saskatoon, our team of radiologists, technologists, and support staff work in a truly integrated way to provide exceptional experiences for our patients. Joining our team is more than a job. It’s an investment in your future — a plan for success.
OUR PEOPLE
Our people share our quest to make a difference in our patient’s lives. We’re a team of professionals, disciplined in our skills and compassionate with our patients, providing the care and attention they need. At our core, we are a trusted partner in our patients’ health care journey. Our patients, physicians, and other health care providers rely on us for quality imaging to help manage their patient’s health care decisions with certainty. But our business is about more than just imaging. It’s about building lasting relationships and making a meaningful difference in the lives of those we meet.
OUR VISION
A world in which every person has clarity about their health. We push the boundaries of what is possible and embrace change as an opportunity. We strive to be thought leaders and encourage creativity by providing a safe place for calculated risk taking. We learn from our mistakes. We share best practices across our operations and are recognized by our peers for our work. We engage the best to help propel us forward in achieving our goals.