TOLL FREE:
1-866-611-2665
Home BREAST CANCER RISK AND BREAST DENSITY: IS AGE A FACTOR?
Like the rest of your body, breast tissue changes with age. Changes in firmness and size are a normal part of aging, especially after menopause.
However, the risk of developing breast cancer increases with age. According to the Canadian Cancer Society, breast cancer will affect one in eight women in Canada. It typically occurs in women between 50 and 69 years of age but can certainly occur in younger age groups.
Some changes to the breast can be a sign of health problems. You should speak to your health care practitioner if you are experiencing any of the following changes to your breasts:
Dense breast tissue increases the risk of breast cancer, especially in older women. For women with dense breast tissue in 75 percent or more of their breasts, their breast cancer risk is double relative to the general population.
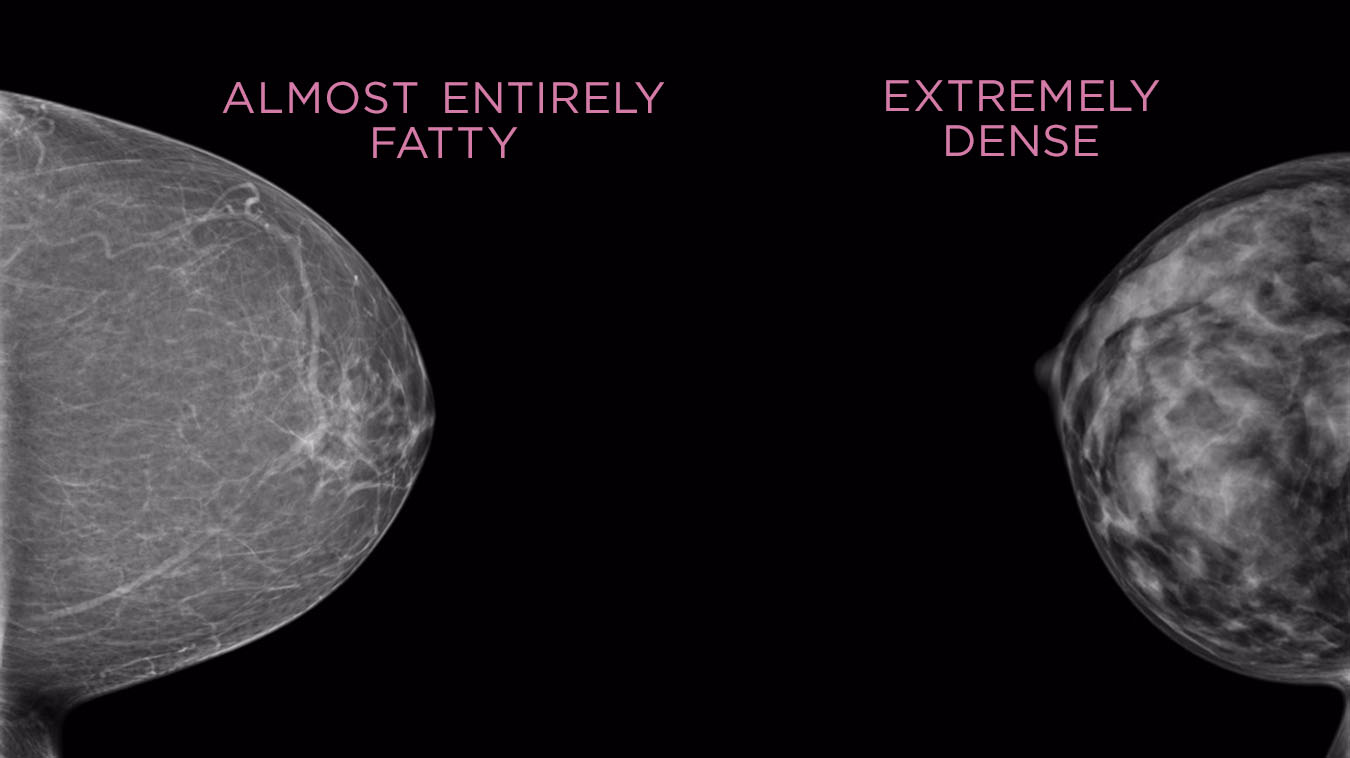
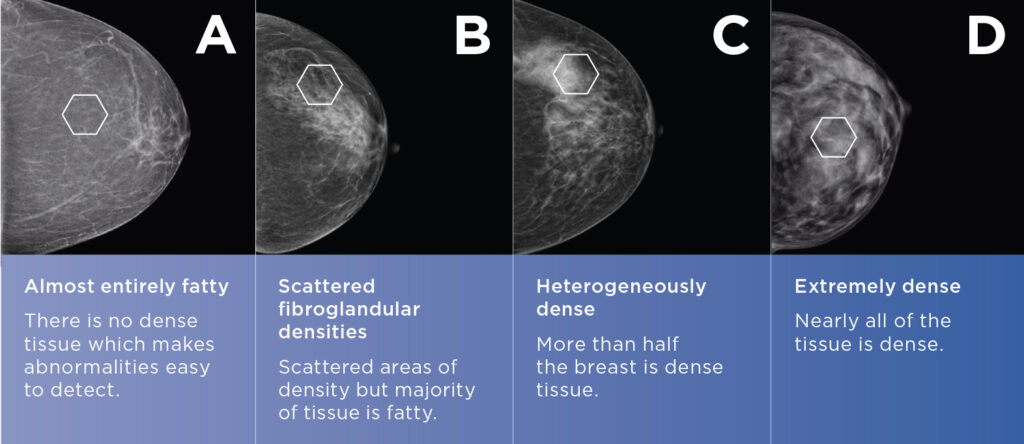
You can’t tell by look or feel whether or not you have dense breasts. It’s a diagnosis that can only be assessed by mammography. Dense breasts have less fat and more glandular and connective tissue. This makes a mammogram harder to read, so smaller cancers may be hidden.
Dense breasts are normal. Breast tissue can change with age, usually becoming less dense as you get older and go through menopause. However, some women continue to have dense breast regardless of age. Dense breasts may be affected by taking certain types of hormone therapies, such as hormone treatments for menopause.
It’s important to be aware of your breast density. At Mayfair, we explain your breast score and include your density level in the report that is sent to your referring doctor. Our mammography machines are equipped with the Volpara Health Technologies program which standardizes the density score from A to D:
The survival rates for breast cancer have been improving since the 1980s, thanks to earlier detection from regular mammogram screening and improvements in breast cancer treatments. When breast cancer is found at an early stage, it’s more easily treated and the survival rate is much higher.
The best way to detect breast cancer early is by having regular screening mammograms before you develop symptoms of breast cancer like lumps, changes to the breast, or even pain in certain instances. This is why educating women about early detection is often the main goal of breast awareness month and its associated fundraisers and campaigns.
Having regular mammograms makes it easier for a radiologist to compare your images and see changes or areas of concern over time. If you wait until you have symptoms, the breast cancer might be enlarged and more difficult to treat.
Mammography is a type of X-ray exam that takes an image of the inside of the breasts. All Mayfair Diagnostics’ mammography clinics provide 3D images (tomosynthesis) of the breast that can then be viewed in slices. This provides a greater level of detail and a clearer view of the breast tissue with a very small dose of radiation – the same level of radiation as 2D images require.
For extremely dense (Volpara D), or heterogeneously dense breast tissue (Volpara C) combined with additional risk factors for breast malignancy, Mayfair recommends supplemental automated breast ultrasound (ABUS) or handheld breast ultrasound, in addition to regular mammograms.
Using both ultrasound and mammograms together helps provide a more complete picture of dense breast tissue. Ultrasound on its own is not recommended as a breast cancer screening tool by the College of Physicians and Surgeons.
All women should have a mammogram. Many women start having regular mammograms every year at about age 40. Alberta Health Care covers one mammogram per year starting at that age. If you have a concern about your breasts earlier than that, you should see your doctor and arrange to have appropriate imaging of your breasts. This may be a mammogram, ultrasound, or both. To get a screening mammogram, you will need to speak to your doctor about your family history, when to start screening, and how frequently you should be screened.
Mayfair Diagnostics recommends screening mammography every year from age 40 to 49, then every two years between age 50 and 74, if there are no risks factors that would necessitate a shorter interval. After age 75, screening frequency will depend on a number of factors, including your medical history.
Women with the following risk factors are considered high risk and may be encouraged to start screening earlier and more frequently:
NOTE: If you are at high risk, Mayfair recommends regular breast screening every year starting at any age above 40 or 10 years earlier than the age a first-degree relative was diagnosed with breast or ovarian cancer.
Across Canada the recommended age to start screening and the recommended screening intervals differ by province. Most provincial and federal breast screening guidelines are based on an evaluation of whether the benefits of regular screening mammograms outweigh the potential harms. Mayfair’s recommendations for breast screening are aligned with the Canadian Society of Breast Imaging and the Canadian Association of Radiologists.
When deciding between the benefit of early detection of breast cancer and the potential harms associated with breast cancer screening there are two main concerns that are often considered. The first is radiation exposure and the second is overdiagnosis.
Many women are concerned about the cumulative effects from radiation exposure during a mammogram. However, mammograms require a very small dose of radiation, less than the annual background environmental radiation exposure. Many women consider the risk of harm from this amount of radiation exposure to be low compared to the prognosis when breast cancer is detected early.
Overdiagnosis includes unnecessary treatment of cancer that would not have caused harm in a woman’s lifetime, as well as the physical and psychological consequences of false positives. Current research puts the risk of overdiagnosis at 10 percent, compared to research that shows not participating in screening mammography leads to a 60 percent higher chance of dying from breast cancer.
While the recommendations differ, the ultimate decision rests with women. Understanding the risks and benefits of regular mammogram screening and speaking with your doctor about your medical history is an important first step to decide what’s right for you.
Mayfair Diagnostics has 14 mammography locations, which have all been updated recently with the newest technology. Thirteen of our mammography locations also feature patient-assisted compression – which helps provide a more comfortable mammogram. Coventry Hills has an upgraded mammography system but doesn’t offer patient-assisted compression.
Automated breast ultrasound is available at our Market Mall, Mayfair Place, Southcentre, and The CORE locations. Please visit our breast imaging services page for more information.
Advani, S. M., et al. (2021) “Association of Breast Density With Breast Cancer Risk Among Women Aged 65 Years or Older by Age Group and Body Mass Index.” JAMA Network Open. 2021;4(8). Accessed September 15, 2021.
Alberta Health Services Breast Cancer Screening Programs (2021) “Breast Cancer Screening.” www.screeningforlife.ca. September 15, 2021.
Canadian Association of Radiologists (2016) “CAR Practice Guidelines and Technical Standards for Breast Imaging and Intervention.” www.car.ca. September 15, 2021.
Canadian Cancer Society (2021) “Breast cancer statistics.” www.cancer.ca. September 15, 2021.
Canadian Cancer Society (2021) “Breast density.” www.cancer.ca. September 15, 2021.
Canadian Society of Breast Imaging (2018) “The Canadian Society of Breast Imaging response to the new CTFPHC Guidelines.” www.csbi.ca. September 15, 2021.
Eske, J. (2019) “How do the breasts change with age and why?” www.medicalnewstoday.com. Accessed September 15, 2021.
Kahn, A. (2019) “Aging Changes in the Breast.” www.healthline.com. Accessed September 15, 2021.
Monticciolo, Dr. et al. (2018) “Current Issues in the Overdiagnosis and Overtreatment of Breast Cancer.” American Journal of Roentgenology. February 2018, 210 (2). September 15, 2021.
Tabar, L., et al. (2018) “The incidence of fatal breast cancer measures the increased effectiveness of therapy in women participating in mammography screening.” Cancer. September 15, 2021.
Our Refresh newsletter delivers the latest medical news, expert insights, and practical tips straight to your inbox, empowering you with knowledge to enhance patient care and stay informed.
By subscribing to our newsletter you understand and accept that we may share your information with vendors or other third parties who perform services on our behalf. The personal information collected may be stored, processed, and transferred to a country or region outside of Quebec.
Please read our privacy policy for more details.
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |